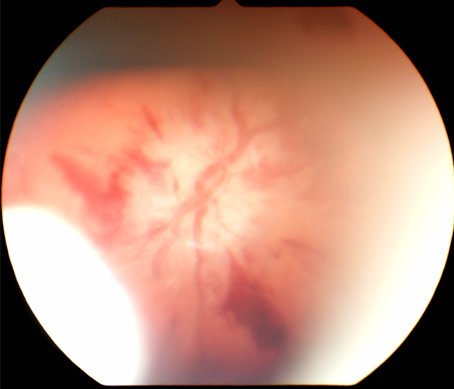
A 4-month-old infant without a history of trauma presents with rib fractures, acute bilateral subdural hemorrhages and the unilateral retinal hemorrhage shown below.
Accessible Version
An ocular photograph of a retina showing the optic disc with blood vessels traversing the disc and others surrounding the disc with multiple areas of leaked blood.
Which of the following is a true statement about this retinal hemorrhage?
◯
A. This finding of a unilateral retinal hemorrhage indicates that inflicted head trauma is unlikely.
◯
B. This unilateral retinal hemorrhage is likely due to birth trauma.
◯
C. This unilateral retinal hemorrhage supports a diagnosis of inflicted head trauma.
◯
D. This hemorrhage is most likely due to increased intracranial pressure.
Which of the following is a true statement about this retinal hemorrhage?
◯
A. This finding of a unilateral retinal hemorrhage indicates that inflicted head trauma is unlikely.
◯
B. This unilateral retinal hemorrhage is likely due to birth trauma.
✓
C. This unilateral retinal hemorrhage supports a diagnosis of inflicted head trauma.
◯
D. This hemorrhage is most likely due to increased intracranial pressure.
The best answer is C
The association of retinal hemorrhages with inflicted head trauma and child abuse is well recognized. Repeated acceleration-deceleration forces of the eye/head, with or without impact, is the most likely etiology in inflicted injury. When inflicted head trauma is suspected, a complete retinal examination performed by an ophthalmologist skilled in pediatric examinations is recommended. It is important to obtain a three dimensional view of the entire retina, preferably through a dilated pupil using an indirect ophthalmoscope, and have accurate descriptions of the hemorrhages.
The hemorrhages photographed in this case show intraretinal bleeding as well as pre-retinal bleeding. This is often described as "multi-layered." The larger hemorrhage near the 5 o’clock position is a pre-retinal hemorrhage. Intraretinal blood that is more superficial and streams along nerve fibers is often described as "flame" or "splinter" retinal hemorrhages. These can be seen in this photograph as well. Deeper intraretinal hemorrhages are often described as "dot" hemorrhages and are not clearly visible in this photo. Further descriptive terms can be reviewed in the suggested references below.
Retinal hemorrhages can be seen in approximately 85% of abusive of head trauma victims. Retinal hemorrhages can occur, less commonly, when there is not evidence of intracranial bleeding.
Unilateral retinal hemorrhages can occur with accidental or non-accidental (inflicted) head trauma. Retinal hemorrhages isolated to the posterior pole of the retina and located on the same side as an intracranial hemorrhage have been associated with accidental head trauma. However, the presence of unilateral retinal hemorrhages does not rule out inflicted trauma.
Birth related trauma may result in retinal hemorrhages. These intraretinal hemorrhages usually resolve within a few weeks. Infants born with vacuum assisted extraction have been reported to have prolonged presence of retinal hemorrhages (up to 58 days in one report). It is rare to see birth related hemorrhages after a few months of age and those that do remain for prolonged periods are residual, discrete hemorrhages. Extensive confluent hemorrhages resolve quickly (days to a few weeks). Although retinal hemorrhages have been rarely reported after Caesarean section delivery, other types of delivery with instrumentation have a higher risk of retinal hemorrhages. The presence of birth- related retinal hemorrhages in a 4 month old, as in this case, has not been reported.
Papilledema from increased intracranial pressure occurs in a very small percentage of cases of inflicted head trauma. This photograph does not demonstrate papilledema. Increased intracranial pressure may play some role in the development of retinal hemorrhages, but there is no evidence demonstrating a clear association between retinal hemorrhages that are "too numerous to count" and increased intracranial pressure in children.
Special thanks to Leon-Paul Noel, MD (Pediatric Ophthalmologist, Syracuse, NY) for review of this "Test Your Knowledge" question.
- Arlotti SA, Forbes BJ, Dias MS, Bonsall DJ. Unilateral retinal hemorrhages in shaken baby syndrome. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2007; 11 (2) : 175-8.PURPOSE: To present a detailed series of patients with unilateral retinal hemorrhages in shaken baby syndrome. METHODS: Patients with a diagnosis of Shaken Baby Syndrome evaluated by the Ophthalmology Department at Penn State University between January 1999 and January 2004 were reviewed. Patients were identified and their medical records, photographs, and computed tomographic scans were reviewed. Additional records were obtained from the Children's Hospital of Philadelphia. RESULTS: Of the 12 patients evaluated at Penn State University, the age at presentation ranged from 6 weeks to 15 months, with an average age of 4.3 months. Six (50%) had bilateral intracranial hemorrhage, while 6 (50%) had unilateral intracranial hemorrhage. The six patients with unilateral intracranial hemorrhage all had ipsilateral retinal hemorrhages. The perpetrators were male (100%) and 11 (92%) were the babies' fathers. For the five patients evaluated at Children's Hospital of Philadelphia, the age at presentation ranged from 4 weeks to 1 year, with an average of 4.35 months. Three (60%) had bilateral intracranial hemorrhage and two (40%) had unilateral intracranial hemorrhage. The perpetrators were male in four (80%) cases and three (60%) were the babies' fathers. CONCLUSIONS: These patients demonstrate the varied presentations of shaken baby syndrome. Unilateral retinal hemorrhages do not rule out the diagnosis of shaken baby syndrome.
- Hughes LA, May K, Talbot JF, Parsons MA. Incidence, distribution, and duration of birth-related retinal hemorrhages: a prospective study. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2006; 10 (2) : 102-6.BACKGROUND: Retinal hemorrhages secondary to birth trauma are part of the differential diagnosis of intraocular hemorrhages seen in the setting of Shaken baby syndrome in very young infants. This prospective study aimed to document the morphology, distribution and, most importantly, the natural history of these hemorrhages using digital imaging. SUBJECTS AND METHODS: Infants were recruited as soon after birth as possible and examined by indirect ophthalmoscopy. Retinal hemorrhages were photographed using the RetCam 120. Birth history was documented from the medical notes. Infants were reexamined and photographed until hemorrhages had resolved. RESULTS: Data were analyzed for a total of 53 neonates. The number of infants with retinal hemorrhage was 18 (34%). The incidence in relation to mode of delivery was as follows: vacuum delivery, 77.8%; normal vaginal delivery, 30.4%; cesarean section, 8.3%; forceps delivery, 30.3%. All hemorrhages were intraretinal and in all but two infants hemorrhages had resolved by 16 days. In two subjects hemorrhages were still present at 31 and 58 days, respectively. Both these infants were delivered by vacuum delivery. CONCLUSIONS: The RetCam 120 provides excellent documentation of retinal hemorrhages and their natural history. We have demonstrated hemorrhages still present at 58 days in a child born by vacuum delivery and this may have important implications for consideration in the differential diagnosis of Shaken baby syndrome.
- Jenny C. Recognizing and responding to medical neglect. Pediatrics. 2007; 120 (6) : 1385-9.A caregiver may fail to recognize or respond to a child's medical needs for a variety of reasons. An effective response by a health care professional to medical neglect requires a comprehensive assessment of the child's needs, the parents' resources, the parents' efforts to provide for the needs of the child, and options for ensuring optimal health for the child. Such an assessment requires clear, 2-way communication between the family and the health care professional. Physicians should consider the least intrusive options for managing cases of medical neglect that ensure the health and safety of the child.
- Christian CW, Levin AV. The Eye Examination in the Evaluation of Child Abuse. Pediatrics. 2018; 142 (2).Child abuse can cause injury to any part of the eye. The most common manifestations are retinal hemorrhages (RHs) in infants and young children with abusive head trauma (AHT). Although RHs are an important indicator of possible AHT, they are also found in other conditions. Distinguishing the number, type, location, and pattern of RHs is important in evaluating a differential diagnosis. Eye trauma can be seen in cases of physical abuse or AHT and may prompt referral for ophthalmologic assessment. Physicians have a responsibility to consider abuse in the differential diagnosis of pediatric eye trauma. Identification and documentation of inflicted ocular trauma requires a thorough examination by an ophthalmologist, including indirect ophthalmoscopy, most optimally through a dilated pupil, especially for the evaluation of possible RHs. An eye examination is helpful in detecting abnormalities that can help identify a medical or traumatic etiology for previously well young children who experience unexpected and unexplained mental status changes with no obvious cause, children with head trauma that results in significant intracranial hemorrhage and brain injury, and children with unexplained death.